Four out of every five breast cancer patients undergo complementary therapies to manage anxiety and stress after they receive a diagnosis.
 A new study conducted by Columbia University in co-operation with several major oncology facilities examined which therapies benefit patients the most. The answer? Meditation and yoga.
A new study conducted by Columbia University in co-operation with several major oncology facilities examined which therapies benefit patients the most. The answer? Meditation and yoga.
Practice guidelines for
medical institutions
The impressively thorough study, published in Journal of the National Cancer Institute Monographs (Oxford University Press), looked at 80 different alternative therapies and covered more than 4,900 clinical trials from the past 25 years.
Therapies were graded with respect to their effectiveness in treating various symptoms.
Overall, meditation (including the Transcendental Meditation technique), yoga, and relaxation with imagery were found to have the strongest evidence supporting their use.
They received an “A” grade and are recommended for routine use for anxiety and other mood disorders common to breast cancer patients.
The same practices received a “B” grade for reducing stress, depression, and fatigue.
The researchers also gave some therapies low grades. For example, healing touch was given a “C” for lowering pain, and aloe vera gel was not recommended at all for preventing skin reactions from radiation therapy.
Conclusion? Patients now know which therapies to go for
Women with breast cancer are among the highest users alternative, non-inventive therapies. The comprehensive study now makes it easier to separate the wheat from the chaff.
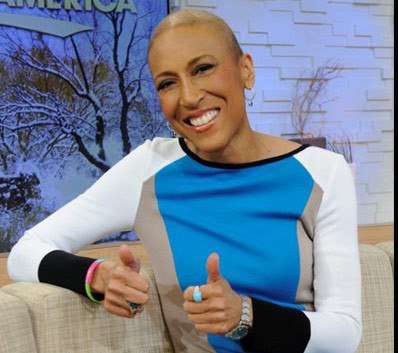
“Most breast cancer patients have experimented with integrative therapies to manage symptoms and improve quality of life. But of the dozens of products and practices marketed to patients, we found evidence that only a handful currently have a strong evidence base,” said lead researcher Dr. Heather Greenlee from Columbia University’s Mailman School of Public Health.
“The published guidelines provide an important tool for breast cancer patients and their clinicians as they make decisions on what integrative therapies to use and not use,” explained Dr. Greenlee, the president of the Society for Integrative Oncology.
“These guidelines clearly demonstrate that clinicians and patients should adopt shared decision-making approaches when assessing the risk-benefit ratio for each therapy. It is important to personalize the recommendations based upon patients’ clinical characteristics and values.”
Full text online:
Greenlee, H. et al. (2014). “Clinical Practice Guidelines on the Use of Integrative Therapies as Supportive Care in Patients Treated for Breast Cancer”. Journal of the National Cancer Institute Monographs. No 50, pages 346-358. http://jncimono.oxfordjournals.org/content/2014/50/346.full